First, thanks for your patience while I took a break last month! I’ve restructured my life and am now building our media company, Red Flag Hero, full-time.
The response to Red Flag Hero has been incredible.
My business partner—who’s spent a decade in startups—often reminds me: the right offer, at the right time, with the right people works. And it’s working. We’ve been partnering with mission-aligned healthcare companies, founders, and executives to create done-for-you social media content that drives attention, impact and growth.
While I’ll miss past projects, I’m beyond grateful to focus entirely on bringing unfiltered, uncompromised conversations about health and healthcare to more people.
We need systemic change and that starts with each of us as individuals.
Full transparency? I’m having a blast.
Now, let’s dive in.
You’ve heard of six degrees of separation—the idea that any two people are connected through just a handful of relationships.
In healthcare, I’d argue it’s more like two or three degrees—because no matter the topic, the conversation always circles back to the same fundamental debate:
Lifestyle interventions (diet, exercise and behavior change) vs. Medicalization (dysfunction becomes ‘diagnosis’ - managed through prescriptions/procedures…etc)
This tension has shaped my entire career—from exercise scientist to researcher to ER clinician. And nowhere is it more apparent than the rise of GLP-1 receptor agonists (like Wegovy and Ozempic) for weight loss.
While their approval has been met with excitement, history warns us to proceed with caution. Many so-called “game changers” have later revealed serious risks—sometimes decades after approval.
Need a reminder? Look at Vioxx—once a blockbuster painkiller, later pulled from the market after causing tens of thousands of deaths from heart attacks.
So I started asking:
What do people who’ve conquered obesity without medication think?What about professionals who’ve guided weight loss journeys for decades?
I went straight to the source.
The Perspective of Those Who’ve Done It Themselves
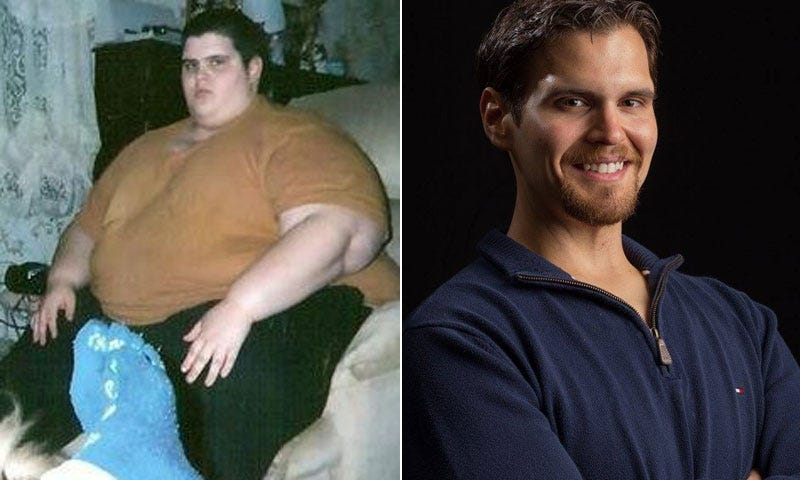
I started by interviewing Justin Willoughby, a podcaster, public speaker and author who lost 600 pounds and made headlines on national platforms like The Today Show, The Doctors and The Huffington Post. His weight loss journey is also chronicled in his book, One Step: How I Took One Step To Lose 600 lbs.
His take?
Lasting weight loss requires a supportive community and a long-term mindset. He believes the human connection piece matters more than we think.
Our full conversation is here.
A Trainer’s Perspective: Fitness ≠ Weight Loss
I also spoke with Durrell Finch, a former trainer to Hollywood’s elite. His concern? The obsession with “losing weight” rather than building health.
He points out the obvious…
“Skinny isn’t the same as fit.”
And he’s right. The people you see on TV that you want to look like, aren’t just ‘skinny,’ they work out. He believes that health requires a more comprehensive approach.
Our full conversation is here.
As a clinician, I want to help people and I’m open to doing that in a variety of ways including for weight loss.
Obesity is a ‘metabolic disease,’ which means it is a dysfunction of the body's ability to process and use energy, nutrients and hormones. It includes issues like insulin resistance and increased inflammation.
Although I’m a huge proponent of personal responsibility, at the end of the day, as a clinician, I don’t care if the patient participated in their disease formation or not. I treat many disorders exacerbated by ‘patient behavior.’ We all do - it’s just part of the practice of medicine.
While personal responsibility is paramount, it’s also important to recognize that there are multiple billion-dollar industries that prosper proportionately to patient suffering.
Health policy can’t be omitted from the discussion.
Think of it this way—
An obese kid is a ‘cash cow’ for Big Food, Big Pharma, Big Insurance, hospitals and the healthcare industry in general. Incentives are aligned to create what is profitable.
Shaming those who simply are susceptible to a system that has been carefully constructed to increase the likelihood of illness, just doesn’t make sense to me. But that does not mean that people are entitled to treatment with GLP-1 medications.
Meds aren’t a miracle fix, and we must acknowledge that there are still far more unknowns than knowns.
While GLP-1s offer an effective way to lower body weight, the long-term health consequences, economic incentives driving their widespread use and the societal failure to address root causes of obesity remain major concerns.
The Risks We Know—And the Bigger Risks We Don’t
Clinical trials show that GLP-1 medications can lead to 10-15% weight loss in a year (only while the drug is being continuously used), but at what cost?
Known risks include:
Belly issues: Nausea, vomiting, diarrhea, bloating
Pancreatitis: A painful and potentially life-threatening inflammation of the pancreas
Gallbladder disease: Increased risk of gallstones and gallbladder removal (common with all quick weight loss)
Thyroid tumors: Found in animal studies, unclear risk in humans
Excessive muscle loss: with potential to contribute further to future metabolic dysfunction and frailty
But the real concern lies in what we don’t yet know.
What happens when patients stop taking the drug? Early data suggests most people regain the weight, which could lead to long-term dependency on medication.
Are there unknown long-term consequences? We saw this with Vioxx, where increased heart attacks weren’t detected until millions had already taken the drug. What unknown risks could emerge with decades of GLP-1 use?
Are the effects on hormones fully understood? We are altering fundamental hormonal pathways related to hunger and digestion—a complex system we do not yet fully understand.
What is the effect on interpersonal relationships and brain function? We are turning down ‘irrational’ or ‘emotional’ behavior, but isn’t that exact behavior that makes us human in beautiful ways?
Despite these uncertainties, the financial incentives for drug companies, healthcare systems and even insurers favor widespread prescribing.
Follow the Money: Why Drugs Get the Green Light While Policy Change Stalls
Pharmaceutical companies clearly have strong incentives to promote lifelong medication use over other interventions like diet and exercise. GLP-1 medications generate billions in revenue and companies benefit when patients stay on them indefinitely.
By contrast, common-sense, low-cost public health measures—like improving school lunches or eliminating soda from government food assistance programs—are consistently ignored. Why? Because they don’t generate profits for corporate interests.
Consider these examples:
School Lunches: The government sets the nutrition standards for millions of children’s meals, yet schools still serve ultra-processed, low-protein, high-carb meals that contribute to obesity. Meanwhile, vending machines stocked with sugar-laden snacks remain in many schools.
Coca-Cola and SNAP Benefits: The Supplemental Nutrition Assistance Program (SNAP), meant to help low-income families access food, spends billions each year on sugary drinks—a major driver of obesity. The soda industry actively lobbies to keep these purchases allowed.
Instead of fixing these systemic problems, we rely on expensive drugs to manage the consequences?
It doesn’t make sense.
Medication Alone Will Never Solve Obesity
Even if GLP-1s help some, they don’t fix the environment that made obesity so common in the first place.
Obesity rates have tripled over the last few decades. Some of the causes?
• Ultra-processed food
• Economic policies that make junk food cheap
• A healthcare system that treats disease, not health
Drugs don’t change any of that.
Here’s the uncomfortable truth:
Until we create an environment where healthy food is affordable, physical activity is accessible and corporate influence over public health is reduced, obesity will persist—no matter how many new drugs hit the market.
So as clinicians, industry professionals, and patients who get it—isn’t it our responsibility to push for real change instead of advocating for yet another band-aid?
The Bottom Line
GLP-1 medications offer short-term weight loss, but at an unknown long-term risk. Before we rush to embrace these drugs as the default solution, we must:
Ask hard questions about safety, long-term outcomes and who stands to gain
Acknowledge that weight loss alone does not equal health
Push for real public health reforms—like better food policies.
We’ve been here before—with Vioxx, with fen-phen and with countless other “miracle” drugs.
The question isn’t whether GLP-1 medications work in the short term—it’s whether we’ll still be using them once we truly understand their long-term effects and what we should be doing to avoid being sick in the first place.
Until next time,
**Never medical advice
Ps. If you found this article helpful, please consider sharing it with a friend. If you want to contribute to the discussion, please leave a comment below!






Great write up! Thinking material for many to consider.
It scares the bajeebies out of me when I see so much press about GLP-1s being a “miracle.”